Cancer treatments have made significant strides over the past few decades, leading to improved outcomes for many patients. However, one of the persistent challenges in cancer therapy is how these treatments interact with the body’s immune system. In particular, a concerning aspect is that many traditional and emerging cancer therapies, while effective in targeting tumors, can inadvertently suppress the T cell immune responses. This suppression can hinder the body’s natural defense mechanisms, allowing cancer cells to evade the immune system.
In this article, we will explore how cancer therapies suppress T cell immune responses, the underlying mechanisms, and the potential implications for cancer treatment and patient outcomes.
Understanding T Cells and Their Role in the Immune System
T cells, also known as T lymphocytes, are a crucial component of the immune system. They play a vital role in recognizing and eliminating cancerous cells, viruses, and other harmful invaders. T cells are primarily divided into two types:
- CD8+ cytotoxic T cells: These are the “killer” cells that directly attack and destroy cancer cells or infected cells.
- CD4+ helper T cells: These assist in activating and coordinating the immune response by signaling other immune cells, including cytotoxic T cells.
T cells are capable of recognizing cancer cells through specific markers on their surface, known as antigens. When functioning properly, T cells can target and eliminate cancerous cells without harming healthy tissue.
How Cancer Therapies Can Suppress T Cell Immune Responses
 While cancer therapies are designed to fight cancer, many of them inadvertently impair the immune system’s ability to mount a robust defense. The suppression of T cell immune responses can occur in several ways, depending on the type of therapy being used. Below are some of the most common therapies and their impact on T cells.
While cancer therapies are designed to fight cancer, many of them inadvertently impair the immune system’s ability to mount a robust defense. The suppression of T cell immune responses can occur in several ways, depending on the type of therapy being used. Below are some of the most common therapies and their impact on T cells.
1. Chemotherapy
Chemotherapy remains one of the cornerstones of cancer treatment. It works by using cytotoxic drugs to kill rapidly dividing cells, including cancer cells. However, chemotherapy also affects healthy cells, particularly those that are involved in immune responses.
Chemotherapy can deplete the body’s pool of immune cells, including T cells. This reduction in T cell numbers weakens the immune system, making it harder for the body to fight cancer or infections. In addition, chemotherapy can alter the function of remaining T cells, making them less effective at recognizing and attacking cancer cells.
2. Radiation Therapy
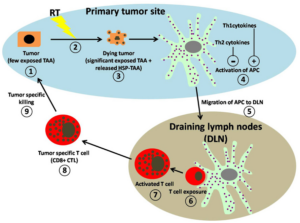
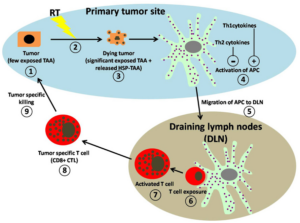
Radiation therapy uses high-energy radiation to damage cancer cells’ DNA, causing them to die or stop dividing. While radiation can be an effective treatment for localized cancers, it also has a profound impact on the immune system.
Radiation can deplete the number of circulating T cells and inhibit their activation. It can also create an immunosuppressive environment by altering the function of immune cells in the tumor microenvironment. In some cases, radiation can even promote the development of immune-checkpoint molecules that suppress T cell activity, allowing cancer cells to escape immune surveillance.
3. Immunotherapy
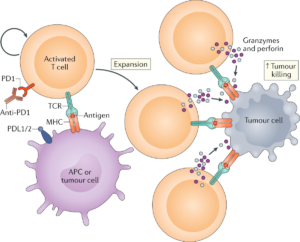
While immunotherapy has shown great promise in enhancing the body’s immune response against cancer, some forms of this treatment can have unintended consequences. For example, immune checkpoint inhibitors, which are designed to block the inhibitory signals that cancer cells use to evade T cell detection, can sometimes lead to immune-related side effects.
In some cases, immune checkpoint inhibitors can cause an overactivation of the immune system, leading to autoimmune reactions where T cells attack healthy tissues. Conversely, some tumor cells can adapt and exploit the immune checkpoint pathways, leading to a suppression of T cell activity despite the presence of immunotherapy.
4. Targeted Therapies
Targeted therapies are designed to interfere with specific molecules involved in cancer cell growth and survival. While these therapies are often more selective and less harmful to healthy cells than chemotherapy, they can still influence immune cell function.
Some targeted therapies can alter the tumor microenvironment, creating conditions that suppress T cell responses. For example, certain molecular targets may lead to the upregulation of immune checkpoint proteins like PD-1 or CTLA-4, which inhibit T cell activation and function. In some cases, targeted therapies may also reduce the expression of tumor antigens, making it harder for T cells to recognize and attack cancer cells.
The Tumor Microenvironment and Immune Suppression
The tumor microenvironment plays a critical role in how cancer cells interact with the immune system, including T cells. Tumors often create an immunosuppressive microenvironment that helps them evade immune detection and destruction.
Several factors within the tumor microenvironment contribute to T cell suppression, including:
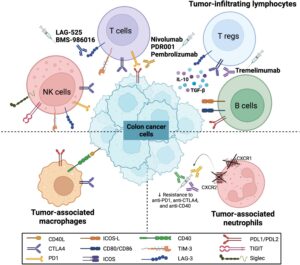
- Immune checkpoint molecules: These are proteins that tumors can express to turn off T cell activity. Common examples include PD-L1 and CTLA-4, which can be upregulated in response to therapy and dampen T cell responses.
- Immunosuppressive cytokines: Tumors can secrete cytokines, such as TGF-β, which inhibit T cell function and promote immune tolerance.
- Regulatory T cells (Tregs): These are immune cells that suppress the activity of other immune cells, including T cells, within the tumor microenvironment.
The interplay between these factors can make it challenging for T cells to effectively attack cancer cells, especially after treatment.
The Future of Cancer Treatment: Enhancing T Cell Responses
While many cancer therapies suppress T cell responses, the future of cancer treatment is focusing on ways to overcome these challenges. Researchers are exploring novel strategies to enhance T cell function, including:
- Combination Therapies: Combining chemotherapy, immunotherapy, and targeted therapies may help overcome T cell suppression. For example, combining immune checkpoint inhibitors with chemotherapy or radiation therapy may help to “re-activate” T cells that have been suppressed by the tumor microenvironment.
- CAR-T Cell Therapy: Chimeric Antigen Receptor T cell (CAR-T) therapy involves modifying a patient’s T cells to express receptors that specifically target cancer cells. This approach has shown success in blood cancers and is being investigated for solid tumors.
- Immune Adjuvants: These are substances that enhance the body’s immune response. Researchers are studying adjuvants that can boost T cell activation and reduce immune suppression caused by cancer therapies.
- Tumor Microenvironment Modulation: By targeting the immune-suppressive components of the tumor microenvironment, researchers aim to create a more favorable environment for T cells to function effectively.
Conclusion
While many cancer therapies have revolutionized the treatment of cancer, they can also have unintended consequences, including the suppression of T cell immune responses. This challenge highlights the complexity of cancer treatment and the need for a more nuanced approach that not only targets the tumor but also supports the body’s immune defenses.
As research continues to uncover the mechanisms behind immune suppression, new therapies that enhance T cell function and overcome immune evasion are likely to improve outcomes for cancer patients. The ultimate goal is to find ways to unleash the full potential of the immune system to fight cancer without compromising its ability to protect the body from other threats.